
By Dr. Michael Avery, Rheumatologist
My patients ask me if there’s anything they can do to make their arthritis better. Their faces light up when I say, ‘Yes, in fact there is.’
I am referring to their diet.
Certain foods have been shown to exhibit anti-inflammatory characteristics based on the compounds of which they are made, all which ease the symptoms of the disease and in turn, ease the pain of the disease. In fact, a 2017 survey conducted by the US National Library of Medicine National Institutes of Health indicated that 24% of those with rheumatoid arthritis reported their diet had an impact on the severity of their symptoms.
Even better news is that the foods that offer anti-inflammatory aid range throughout the food groups, so those who suffer from arthritis are sure to find something that will please their palettes while helping ease their arthritis pain.
Fish
 Certain types of fish are packed with inflammation-fighting omega-3 fatty acids, including salmon, tuna, trout, mackerel and herring. Experts recommend at least 3 to 4 ounces of fish twice a week to help ward off inflammation.
Certain types of fish are packed with inflammation-fighting omega-3 fatty acids, including salmon, tuna, trout, mackerel and herring. Experts recommend at least 3 to 4 ounces of fish twice a week to help ward off inflammation.
Soy
Soy carries the same inflammation-battling omega-3 fatty acids as fish, but without the fins. Soybeans, tofu, and edamame are a few examples of anti-inflammatory soy.
Oils
Extra virgin olive oil and walnut oil are at the top of the list for fighting inflammation in the oil category. Extra virgin olive oil is packed with oleocanthal, which has a make up similar to non-steroidal, anti-inflammatory drugs. Walnut oil is loaded with omega-3s.
Tart Cherries
 Cherries are particularly helpful in reducing the frequency of gout flares. Anthocyanins in cherries, which also give cherries their color, have an anti-inflammatory effect. Anthocyanins can also be found in other red and purple fruits like strawberries, raspberries, blueberries and blackberries.
Cherries are particularly helpful in reducing the frequency of gout flares. Anthocyanins in cherries, which also give cherries their color, have an anti-inflammatory effect. Anthocyanins can also be found in other red and purple fruits like strawberries, raspberries, blueberries and blackberries.
Broccoli
Broccoli, Brussels sprouts and cabbage are all rich in vitamins K and C. As part of the cruciferous family, they are also full of a compound called sulforaphane. Sulforaphane helps slow cartilage damage in joints due to osteoarthritis. Broccoli is also rich in calcium, known for its bone-building benefits.
Green Tea
Green tea is loaded with polyphenols, antioxidants believed to reduce inflammation and slow cartilage destruction. Epigallocatechin-3-gallate (EGCG) is another antioxidant in green tea and is believed to block the production of molecules that cause joint damage.
Fruit
Citrus fruits – like oranges, grapefruits and limes – are rich in vitamin C. So are strawberries, kiwi, pineapple, and cantaloupe. Eating these foods helps prevent inflammatory arthritis and maintain healthy joints.
Beans
Beans help lower C-reactive protein (CRP) in the blood, which rises in response to inflammation in the body. Red beans, kidney beans and pinto beans are especially beneficial to lowering CRP.
Garlic
 Garlic, along with onions and leeks, are part of the allium family. Studies have shown that people who regularly ate foods from the allium family showed fewer signs of early osteoarthritis. Researchers also believe the compound diallyl disulphine found in garlic may limit cartilage-damaging enzymes.
Garlic, along with onions and leeks, are part of the allium family. Studies have shown that people who regularly ate foods from the allium family showed fewer signs of early osteoarthritis. Researchers also believe the compound diallyl disulphine found in garlic may limit cartilage-damaging enzymes.
Ginger
Gingerol is the main bioactive compound in ginger and is responsible for much of its medicinal properties and anti-inflammatory effects.
It really comes down to eating healthy foods. Working some of the anti-inflammatory fruits, veggies, spices and fish into your diet can have a positive effect on your arthritis symptoms and on your arthritis pain. Eating these foods also can help you lose weight, which helps take pressure off the joints. You’ll feel the benefits with your arthritis and your overall health.
Dr. Avery is a Rheumatologist who sees patients at the OSMS Rheumatology and Infusion Therapy Clinic in Appleton and Green Bay.
The post 10 Foods for People with Arthritis appeared first on OSMS - Orthopedic and Rheumatology Services in Wisconsin.
 Before I tell you about my day when I have infusions, here is a little about me. I’m 13 years-old and was diagnosed with Poly JIA (Polyarticular Juvenile Idiopathic Arthritis) a year and a half ago. I am a very active teenager and my hobbies include playing saxophone, flute, soccer, gymnastics, and running. My favorite saying that I try and live by is “Impossible stands for I’m Possible.”
Before I tell you about my day when I have infusions, here is a little about me. I’m 13 years-old and was diagnosed with Poly JIA (Polyarticular Juvenile Idiopathic Arthritis) a year and a half ago. I am a very active teenager and my hobbies include playing saxophone, flute, soccer, gymnastics, and running. My favorite saying that I try and live by is “Impossible stands for I’m Possible.” I love infusions because they help me and I only spend a few hours in the doctor’s office every seven to eight weeks. I feel tired for the first day, but my energy is back then. One to two weeks before my next one I can feel it wearing off. I’m so glad I get infusions at a doctor’s office because:
I love infusions because they help me and I only spend a few hours in the doctor’s office every seven to eight weeks. I feel tired for the first day, but my energy is back then. One to two weeks before my next one I can feel it wearing off. I’m so glad I get infusions at a doctor’s office because: Walking
Walking Yoga
Yoga “Nothing was healing or feeling better,” Mira says. “We didn’t know what was wrong, and then all my joints started to get swollen and started hurting so, Dr. Hein referred me to Dr. Tuttle.”
“Nothing was healing or feeling better,” Mira says. “We didn’t know what was wrong, and then all my joints started to get swollen and started hurting so, Dr. Hein referred me to Dr. Tuttle.” She continues, “The hardest part is I don’t look sick. I don’t have a cast or brace on so it is not obvious. Sometimes people don’t understand why I can’t stand or sit in the same position for a while or understand that I am in pain.”
She continues, “The hardest part is I don’t look sick. I don’t have a cast or brace on so it is not obvious. Sometimes people don’t understand why I can’t stand or sit in the same position for a while or understand that I am in pain.”

 Can CBD help with my arthritis pain?
Can CBD help with my arthritis pain? 
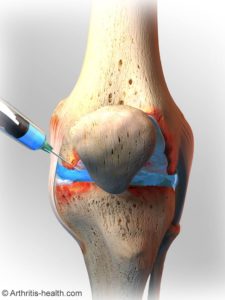
 Osteoarthritis: Causes and Conservative Treatments
Osteoarthritis: Causes and Conservative Treatments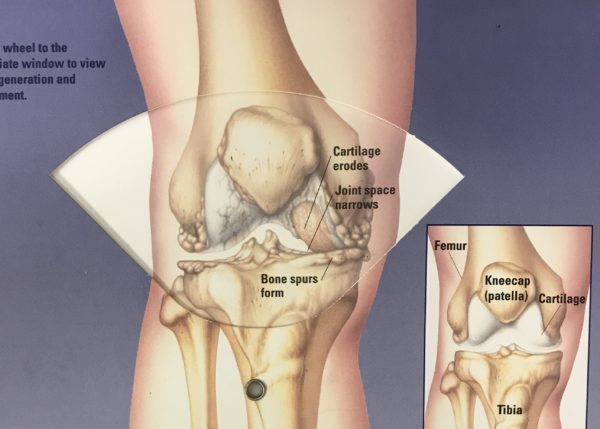
 Add less new frequent joint pain for those with knee osteoarthritis. A recent study published in Arthritis & Rheumatology led by researchers out of Baylor College of Medicine indicates that “walkers” (labeled as such for 10 or more instances of walking for exercise) 50 years and older diagnosed with knee osteoarthritis experienced less new frequent knee pain than “non-walkers” (those who reported less than 10 instances of walking). Once the results were tallied; walkers have a 40% less chance of developing new frequent knee pain compared to non-walkers.
Add less new frequent joint pain for those with knee osteoarthritis. A recent study published in Arthritis & Rheumatology led by researchers out of Baylor College of Medicine indicates that “walkers” (labeled as such for 10 or more instances of walking for exercise) 50 years and older diagnosed with knee osteoarthritis experienced less new frequent knee pain than “non-walkers” (those who reported less than 10 instances of walking). Once the results were tallied; walkers have a 40% less chance of developing new frequent knee pain compared to non-walkers. “This is important information that all OSMS patients should know, particularly our knee osteoarthritis patients, states OSMS Board-Certified Rheumatologist,
“This is important information that all OSMS patients should know, particularly our knee osteoarthritis patients, states OSMS Board-Certified Rheumatologist, 






